By Bello Hussein Adoto
03 December 2023 |
2:00 pm
Last week, the world celebrated Antimicrobial Resistance Awareness (AMR). The goal was to raise awareness about AMR — a phenomenon where antimicrobials no longer kill or prevent the growth of the microbes they used to kill. Our bodies do an excellent job of containing viral, bacterial or fungal infections before a doctor chips in with…


Last week, the world celebrated Antimicrobial Resistance Awareness (AMR). The goal was to raise awareness about AMR — a phenomenon where antimicrobials no longer kill or prevent the growth of the microbes they used to kill.
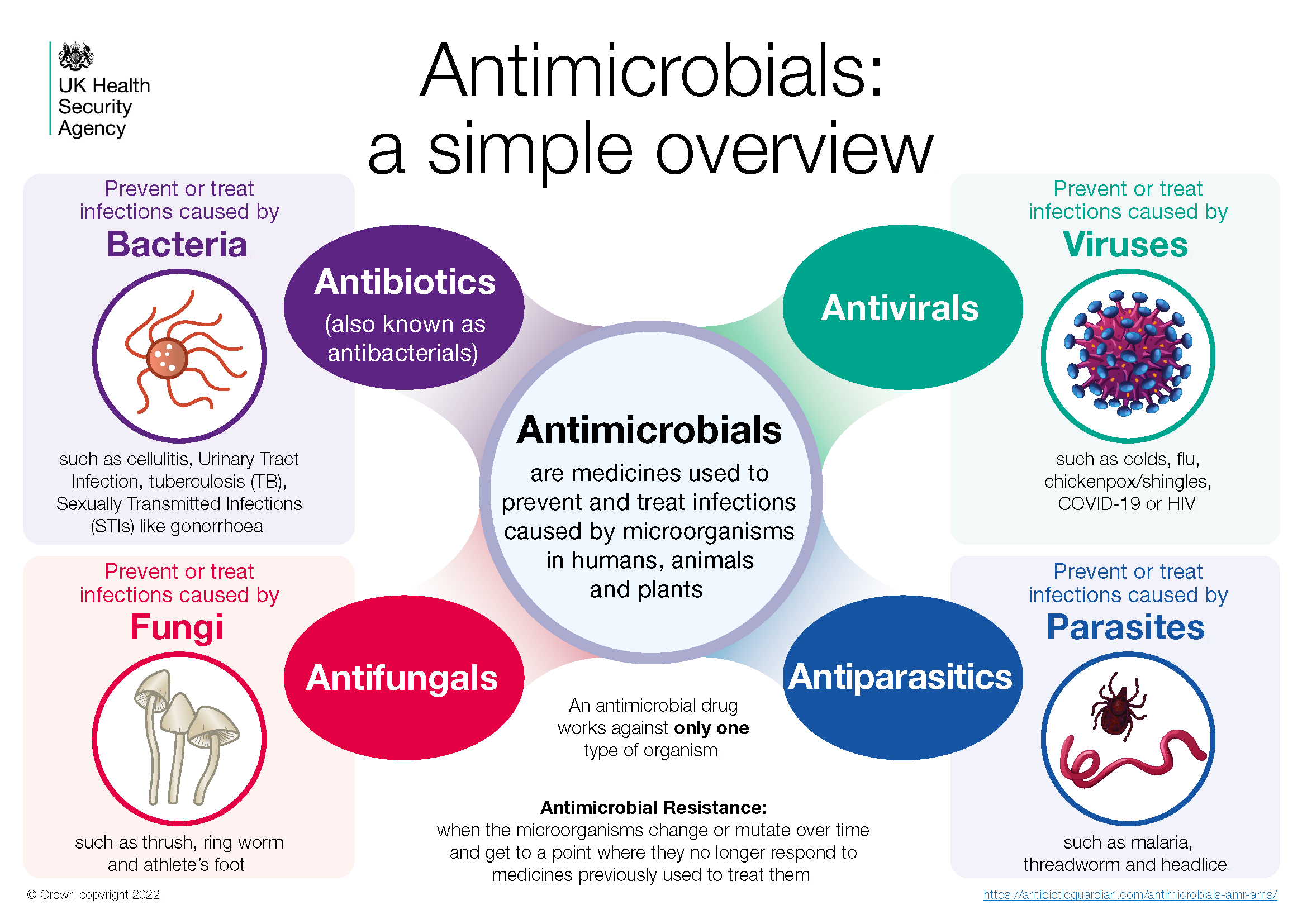
Our bodies do an excellent job of containing viral, bacterial or fungal infections before a doctor chips in with a drug or two to kill the germs and bring us back to good health. These drugs include antibiotics for bacterial infections, antifungals for fungal infections, and antivirals for viral infections.
Unfortunately, some of us don’t go to — or wait for — the doctor to treat actual or presumed infections. We dash to the nearest chemist to buy ampicillin over-the-counter for boils (skin abscesses) and amoxil for typhoid. Patients who can’t tell the difference between dysentery and diarrhoea would buy branded Ciprofloxacin or Amoxiclav to resolve prolonged toilet troubles and stomach pain. Those who are not that buoyant would manage metronidazole.
Our health practitioners also contribute to the problem. A survey of 12 countries shows that Nigeria has the third-highest percentage of antibiotic prescriptions. Three out of every five patients on admission at our hospitals are on antibiotics. This heavy use of antibiotics contributes to Nigeria’s AMR burden.
The consequence of our use, abuse, and misuse of antibiotics is that the viruses, the bacteria, and the fungi have grown tough—they no longer fear us and our drugs. Our pills and creams are no longer as effective. Regular bacterial infections that were once treatable with first-line antibiotics have become stubborn. You may need a second or third line to treat them. Diseases that needed only Ciprotab now call for Ceftriazone and Imepenem. Diseases that were once tolerable have become debilitating, if not deadly.
The World Health Organisation (WHO) recently spotlighted the story of a woman who had reconstructive facial surgery following an accident. The wound got infected and they treated the infection only for it to rebound and eat away at her face. Gradually, her facial muscles turned to cheese. Further tests showed she had MRSA, the dreaded methicillin-resistant Staphylococcus aureus. Luckily, the woman survived. “If I’d known earlier, maybe I wouldn’t have lost huge portions of my face,” she said years later.
Our ignorance about AMR doesn’t make it any less deadly. About five million people died from drug-resistant infections in 2019. More than one million of these deaths were linked directly to AMR.

Aside from being deadly, AMR is expensive. Infections with drug-resistant bacteria, for instance, mean that patients spend more on higher and more effective antibiotics. These antibiotics don’t come cheap. Augmentin, one of the go-to drugs for severe infections, is now N13,000. That’s more than one-third of the minimum wage.
The task before us is to stem the tide of this menace. The government is playing its part. It has drawn up a national action plan for AMR. The plan seeks to increase awareness about the problem, promote surveillance and research, and improve access to genuine antibiotics. Doctors also have concepts like delayed prescription and antimicrobial stewardship to guide their prescriptions. You can join the fight too.
One, don’t use antibiotics without prescriptions. Trust your doctors when they say you don’t need antibiotics. Some viral infections like colds can resolve without drugs.
Two, complete your doses when using prescribed antibiotics. It could be tempting to abandon your drugs at the first sign of relief. It could be valid even: some research has shown that extended use of antibiotics after symptomatic relief doesn’t make any significant difference in recovery. Still, don’t discontinue your drugs at a whim. Speak with your doctor.
Also, don’t share antibiotics or prescribe them to others. This should go without saying, but our desire to help friends and loved ones often pushes us to share drugs like antibiotics with them. You can do better by directing your friend or relative to a doctor. Antibiotics are not emergency drugs that can’t wait for a prescription.
Good hygienic practices can help, too. They limit the spread of infections and the consequent antibiotics (ab)use. Wash your hands regularly. Adopt proper etiquette when you are in a hospital or laboratory environment. Doing otherwise increases your risk of contracting or transmitting new infections to your loved ones.
Five, get vaccinated. Vaccines protect you from contracting potentially resistant infections or spreading them to others. Moreover, viral infections that can be prevented with vaccines, like measles and influenza, are some of the reasons people abuse antibiotics. You won’t feel the need to abuse antibiotics when you don’t contract influenza or measles.
The AMR Awareness Week has come and gone, but the problem and its consequences remain. They affect us all; everyone can and should contribute to the solution. You can be a part of the fight by not abusing antibiotics or demanding that your doctor prescribe antibiotics for you when you don’t need them. You can join in by not abandoning your treatment or sharing your drugs. You can get vaccinated too. Start now. Start today. Join the fight against AMR.
 Top Naija News – Nigeria News, Nigerian News & Top Stories Top Naija News – Nigerian Newspapers, Nigerian News. topnaijanews is a daily Nigerian newspaper covering Latest News, Breaking News, Entertainment, Sports, Lifestyle and Politics.
Top Naija News – Nigeria News, Nigerian News & Top Stories Top Naija News – Nigerian Newspapers, Nigerian News. topnaijanews is a daily Nigerian newspaper covering Latest News, Breaking News, Entertainment, Sports, Lifestyle and Politics.